
Yesterday as therapy session with my 3-year old client diagnosed with Attention Deficit Hyperactivity Disorder (ADHD) with accompanying speech and language deficits was just about to start, the parent of my kid from the previous session just arrived and I had to give her feedback on how her child performed during our session.
So before heading out of the therapy room to talk with my other kid's mom at the reception area I told my kid with ADHD:
"I will go outside for a while, okay? But while I'm out I want you to stay seated and keep quiet inside. Don't go outside the room and don't grab anything."
Then while he was seated in front of the table I left him something to monitor his behavior.
"Look, I will leave you this paper. It has a big face on it. But it doesn't have a mouth yet. Later when I get back and I see that you're still sitting down and quiet, I will draw a smile on its face. But if you don't follow, I'll draw a sad face instead, okay?" And he nodded.
So while I was out discussing with the mom of my other kid, of course I'm still a bit weary with how the other kid is doing inside the room with no one and without anything to do - and with just a drawing of a circle and two-dot eyes to oversee him. Even though I had asked another colleague to keep an eye on him from afar in case he wander around, this is going to be a big test for his impulse control and I was wondering if he can make it through. But I wouldn't be surprised if I get back inside the room with all the toys scatterred all around or worse, he has gone outside the room and has ran towards me because he couldn't wait that long. I've seen this kid for only three sessions prior and he was really really hyperactive and impulsive during the initial evaluation.
After 5 minutes or so, I went back inside the room and found him just quietly sitting and looking at the face I had drawn. Everything is in its place and there's not a single mess or clutter that's not already been there. I've done this smiley test technique I invented myself a couple of times before and it still surprises me how it works each time. As a reward, I drew him the well-deserved smiley face he had patiently waited for.
It has always amused me how the smiley face affects us in so many ways. We feel like a single text message when ended with a smiley face is more sincere. A statement written with an accompanying smiley face suddenly becomes positive and encouraging. The use of smiley face has also proven really useful in Occupational Therapy as positive reinforcement, not just for toddlers but for school-aged children as well; not just for children diagnosed with developmental or behavioral conditions but even with regular or normally developing kids.
According to Cecil Adams (1993), the ubiquitous "smiley face" we know - two-dot eyes, and an upward curve on a yellow circle was originally invented by Harvey R. Ball in Worcester, Massachusetts around 1963 to boost the morale of their workers after the merging of two companies. It was a big hit then and the fad lasted for a year or so. Up to this date, we still see commercialized smiley faces, some like exact replica, and others of some various derivatives.
At therapy sessions, kids go gaga over smiley faces. Even the most hyperactive and defiant kid would give anything just to be rewarded with a smiley face. So, how can the iconic silly-looking yellow-faced grin have such a powerful effect?
Dating as far back as in the olden days, we've always associated a smile as something positive. We feel happy, recognized, appreciated or at times, special and important, whenever we receive one.
Throughout life, we've always worked hard for a smile. We feel all giddy when our crush smiles back at us. We feel good when someone shots us a full-faced grin. Even when traveling in a strange place, when you smile at a stranger they automatically smile back at you and thus breaking the ice or any cultural barrier there is. Later on, the smile just evolves into a pat on the back, a high five, words of affirmation, or tangible gifts.
According to an article entitled: "Why do we smile?", babies usually start smiling, blinking and crying as early as the 26th week inside the womb but after birth, infants wouldn't smile until they are 6 weeks old - after they have finally adjusted with the difference in environment outside. This further suggests that smiling is a reflex to positive feelings - of happiness, stability and security.
Later on a child begins his early cognitive development in dichotomy. He only recognizes good and bad, pretty and ugly before he begins to understand gray areas. This somehow explains why more often that not we find babies staring or smiling at more pleasant-looking people and crying at less good-looking people for no apparent reasons.
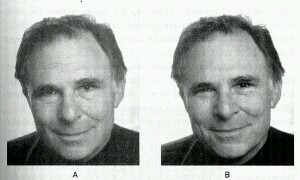
But a "smiley face", as we know, is not real and nothing but a mere representation of anything positive. Scientists have long been studying about the different biological processes related to specific social events - and one of particular interest is that of Guillaume Benjamin Amand Duchenne, otherwise known as Duchenne de Boulogne, a French neurologist who coined the term "genuine smile" or the "Duchenne smile." According to Duchenne, a smile is activated by contractions of various muscles of the face such as the zygomaticus major and orbicularis oculi pars orbitalis. When the zygomaticus major or the muscles at the corners of our mouth contracts, it forms what we call "Pan American smile" or the social smile (see A, image below). When the orbicularis oculi or the muscles around our eyes contracts along with the zygomaticus major then it forms the "Duchenne smile" or the "genuine smile" (see B, image below). Duchenne reiterated that "mouth corners" only smiles are fake and a real smile should involve the eye sockets and mouth corners muscles. A genuine smile is believed to be produced as a result of a positive genuine emotion and is primarily involuntary whereas a Pan American smile is partly voluntary.
Bottomline is: a real smile or not, a visual representation or a face-to-face interaction, a smile is perceived by the brain as something positive. Not only does it make us feel good when we're the one at the receiving end, it also makes us look good when we're the one smiling at others. Smiling also contributes to the general well-being of a person as numerous studies have already proven that those who smiles more live the longest. So make it a habit. After all, it's free. :)
References:
"Smiley face." (2013). Retrieved on August 14, 2013. Http://www.straightdope.com/columns/read/961/who_invented_the_smiley_face
"Smiling." (2013). Retrieved on August 14, 2013. Http://www.serendip.brynmawr.edu/exchange/node/49
"The science of smiling." (2013). Retrieved on August 14, 2013. Http://blog.bufferapp.com/the-science-of-smiling-a-guide-to-humans-most-powerful-gesture
Occupational Therapy
-
Just SMILE: The Real Deal Behind the Ubiquitous Smiley Face and the Science of Smiling
-
Haaay BUDOY... [a review]
When “Budoy” was first aired, I was so happy to learn the fact that, finally, the media is paying more attention to what could be a rapidly growing problem in our society today – the increasing number of kids and individuals who have developmental delays of various causes. I’ve been practicing Occupational Therapy for more than 3 years now and I’ve handled different cases of children and adults with special needs – from autism, ADHD, cerebral palsy, mental retardation to adults with physical and psychiatric conditions. To have a teleserye that empathizes with a lot of parents and families with kids with developmental disabilities would be a great help in rising awareness to those who would resort to confining their loved ones with mental retardation at home for life, or even wasting several years in “denial” then later on deciding to act on it only to find out there’s so much more they could have done years before.
Only to my dismay when instead of what I thought would be like the film “Oasis” or “I Am Sam”…or even something like House MD or Grey’s Anatomy, if I would dream big. Budoy is starting to be more like a fantaserye to me now.It was so disappointing that they didn’t conduct a thorough research when they attempt to deal with medical cases. Gerald Anderson’s acting ability is unquestionably very plausible, the way he deliver and portray a mentally challenged individual. It’s primarily the loopholes in the script and story line that is making this television series not as excellent as to what it could have been.
If I would watch Budoy as a medical professional, I’d look for the big details they missed out such as, Budoy‘s exact medical diagnosis. Now that the character Budoy found out that he came from a rich family, they could have tried all medical interventions a mentally challenged individual might need (and a medical doctor would always recommend) say, Occupational Therapy and Special Education. It would have been better if from there, they gradually habilitate Budoy to be a more functional individual, instead of miraculously making him so smart right after he incurred a coma from a lightning shock. Who are they kidding? Moreover, the story is more focused now in the sibling rivalry and love triangle among the characters.
Now the even greater problem remains…how the parents with children with mental retardation and developmental delays perceive Budoy. I have parents constantly asking me, “teacher paglaki ba ng anak ko magiging katulad din ni Budoy?”… “ibig sabihin teacher may pag-asa ring tumalino yung anak ko kahit nadiagnose with severe MR?” And so, I go on and on explaining to them… Budoy is a fictional character. What works with somebody might not necessarily work for everybody. It’s always best to consult your developmental pediatrician or doctor regularly. Collaborate with your child’s SpEd teachers and therapists as to how to follow-up treatment at home. Above all, always be vigilant to the changing needs of your growing child.
-
Life after graduation
Alas! I finally have the time to sit back, think of all the years that gone by…update my blog (darn, after like what – gazillion years! Nah,, just an overstatement..;p) here I am, alone, doing my regular “reflections..” Indeed, it kind of help me a lot applying all those “thinking back”, reflecting over the things I had done…and had not done, or was not able to do so due to a number of reasons; making a sense out of my shallow life.
In my life now, transition is really a big word. At first I was wondering how I would ever get out into college life struggles, not because I did not enjoy my college life, but the hours and hours I spend inside the four corners of our classrooms get longer and longer.. and it only gets harder every time. Now that I am finally out of it all, I wonder, what now?
I always find myself stuck on one corner of my room...looking back…I never understand why it feels so great to reminisce all those memories of younger years until I realize why - simply because those are the days when everything was better.
Now that I’m beginning the life of a working individual…I’m having a lot of apprehensions.. First, should I work and use my diploma? Or should I use my diploma and work? Haha! What I really mean is that, I know some of my classmates who’d resort to working in a call center instead of using everything they have learned to do what they ought to do…to practice what they really worked hard for, and most importantly, to help other people.
I was grateful and I really appreciate everything that I learned from internship. Not only did it help me apply all the theoretical knowledge we have learned from our lectures and discussions but I also get to mingle with different kinds of people…and learn from them. Internship has taught me a lot of things – from the “what-to-dos” to “what-not-to”. I had the opportunity to get along with various kind of people – from my colleagues to the parents and caregivers and patients with which we offer our services.
It’s amazing how I do this technique and then it works in an actual patient, you realize, hey that’s evidence-based practice. Haha! One example of which was when I handled a 60-something year-old patient with Parkinson’s disease. I was pretty amazed by how I see before my eyes how a cog-wheel rigidity looks or feels like, how a masked fascies looks like, how an intention tremor differs from resting tremor, and the like…stuff I only get to read from books before; and a lot more conditions I got to handle that I was only able to hear and read from medical books and online reference materials.
A big bulk of what I learned was on how to relate with other people. I admit I was never that loud or outgoing person. I was rather shy. But an experience from one affiliation center served as an eye opener for me. I remember one professional that I worked with told me, “kailangan marunong kang makisama sa mga magulang ng mga pasyente…kasi sila ang maaaring makatulong o makasira sayo..” Indeed it’s true. For me, OT as a profession, lives on because of: the parents/caregivers who trust you, and the occupational therapist who has the skills and competency to practice. Establishing rapport is not that difficult for me. I have learned along the way how to interact and get to the level of my kids and their caregivers. But to stay in the profession means you have to be tough. One life-changing incident that could almost crash down my level of self-esteem was when I worked with my colleagues (who were supposed to grade me for my performance), thought we got along well but then all of a sudden, they failed me for reasons I never understood. For one thing, you cannot make all people like you. Even if I grew that way, that I always get what I want…I never argued with anyone or had a fight with someone before…no matter what you do, or how goody-two-shoes you are, you cannot please everyone. And sometimes, you just have to bear with that. If you’d get yourself affected, you’ll only suffer. You’d only prove them that they are right all along. The best counter-attack is to always do the best that you can, prove to them what your real worth, and never settle for a substandard or “okay” performance. When in every circumstances you have the chance to shine and leave a mark. Fortunately, I got the sympathy of my clinical supervisor, he believed in my potentials and he took my side. I couldn’t put into words how thankful and how grateful I was of him then. Coming from a different university than us, I thought he would be bias and all, but then, he fulfilled his job as a clinical supervisor – fair and objective when it comes to all his interns no matter what school they come from.
I remember when another clinical supervisor from one of our affiliation centers talked with me personally about my strengths and weaknesses as an OT. One thing that really marked to me then was when she said, “I think you have the skills…you just have to get out of your nutshell..” I never really understood what she meant until I was undergoing this volunteership program that I applied for to keep me busy during summer, while I was reviewing for the boards this July and my menthor reiterated that to me. Sometimes, it really helps when you have that someone who would make you realize what’s lacking, and what you already have that you need to polish. I know what we have learned and practiced during internship was not enough, and it’s not an excuse that you are not able to give your best shot. I was talking with one parent one time and she was asking me of the summary of the re-evaluation I had done for her child. I was not able to make the summary of re-evaluation because it was no longer required of me by my clinical supervisor since it was only a make-up duty. The parent told me, “hindi mo naisip na kailangan ng anak ko yun pag magpapacheck-up kami sa doctor..” Although it was stated in a manner as a joke, I felt terrible. She has a point. I was no longer doing this to graduate…I am now doing this for my patients. I admit, at some point in my life, I was also like the others who were conscious of their grades…to meet the deadlines of their papers… and what gets compromised? The quality of the service you deliver. It feels sad seeing patients not improving…just because their treatment was not well planned and carried out. Why? Because there’s a rapid transition (not even a transition) or change from one intern to another and kids find it difficult to adjust that’s why they regress; because every OT intern has a different treatment plan from the other even though they handle a similar kid; because the OT intern’s priority is: “basta matapos lang..” Duh, patients are not guinea pigs of the internship, they are people seeking for help and because they get there, found you, they deserve at least a decent intervention to address their problems properly! Who cares if you have no or little make-up days? who cares if you have an average of 1 or 2 in your transcript? Parents don’t have to know your GWA every time they’d walk into the clinic. What they see is your performance, how you handle their kids, and how their child improves even at home because you offered them the help they needed.
I am not saying all these because I do very well in my craft. I, as a practicing OT in the future, have my own flaws and inadequacies. This doesn’t mean that I’d stop here once I realized what’s wrong for we always have the option to do better every time. And before you know it, you’ll feel that you are really happy once you realized that everything is in its place…and a major part of it is because of YOU. -
Psyche Case Story
THE CASE OF A. C.
During my fieldwork at NCMH, I was able to handle a 40-year old, female patient with schizophrenia of undifferentiated type. We were not informed of the diagnosis of the patients at the start of the session so as I was going on with the interview; I relied solely on my observations and on my pre-conceived notions about mentally ill individuals. It was in fact difficult to determine the case of my patient per se because in one look, you wouldn’t actually notice anything wrong about her. She has no delusions or hallucinations. She wasn’t aggressive at all, and there weren’t even any hint of flight of ideas or loose association of thoughts. Her mood was euthymic and her affect was appropriate. The only clue that gave her away was the fact that she was actually staying in a mental institution. It was only after I had gone through history-taking that I noticed some discrepancies in the information she provided as compared to that contained in her medical charts. It was documented in her charts that she was 40 years old, single and was admitted in the year 1998. Contrary to what she told me that she was 39 years old married with a 15-year old son and was admitted on 2002. I was asking myself then, was it a question of orientation or deficits in memory? Or was it her reliability as an informant? Since there wasn’t any caregiver/family member present at the time the interview was conducted to compare the information gathered.
Throughout the interview and the evaluation session, I kept wondering, was it a case of MDD or schizophrenia?what type then? Occupational therapists don’t make diagnoses, that I know, so medical diagnosis given before hand will be very useful. But in cases such as I had encountered, I tried to recall all my stored bulk of information about psychiatric conditions from the back of my mind to help me figure out what to do in the evaluation. There wasn’t stated an exact or clear cause of her condition except that client sustained a fall from the rooftop to the ground a couple of years ago and I presumed it to have contributed to the etiology of the disorder. I know that schizophrenia is idiopathic in nature. At the end, I verified my speculations to be true. My client told me that the barangay officials of their town brought her to NCMH when she was seen wandering aimlessly around the streets for days. She admitted that none of her family in Parañaque, even her relatives in the province knew where she was, of what had happened to her and what has been going on with her now. It was a bit disheartening but then, one must not be overridden by emotions.
Client stated that her primary goal is to get back to her previous work as a helper and a nanny to a one-year old child. This sort of served to be my first dilemma. I’ve decided that my target for treatment would be reality orientation and prevocational skills training since these cater her goals for intervention but I realized that there’s a lot of factors that I need to consider in coming up with these goals. First, if ever I should decide to target prevocational skills training for reintegration to work, will there be a possibility for discharge in the first place, and when? I know it is not unlikely since client has already established near-normal level of functioning. The question would then be, supposing the client will be discharged soon, will she still have a home to get back to considering almost 9 years had lapsed and that none of her family nor relatives ever knew where she was and what happened to her? Considering also her age and history of psychiatric illness, would there be a sound opportunity to get back to her work or at least to be able to work again? The OT diagnosis I formulated then was difficulty in participating in work secondary to impaired process skills associated with schizophrenia, undifferentiated.
When I evaluated my client, I hardly found predominant problems with her participation in occupations. Our clinical supervisor was right when she said that the more functional the client, the finer the problems and the more we’ll have to dig deep to understand the client’s context of occupational performance. No problem was noted in the COPM. She has already established fair working behaviors. Her MSE results were mostly good except in the visuospatial ability and insight part, and some noted deficits in her remote memory. Client generally has intact cognition and sensorium. Upon administration of Interest Checklist, client’s preference of activities helped me decide as to what intervention strategy that I should use that would best suit her. I was aiming then of providing her a task-oriented activity that is just-right and motivating for her age, at the same time, incorporating reality orientation techniques and relearning of prevocational skills. Client has a good potential to be reintegrated back to community and to return to work considering her strengths: intact cognition; good orientation to time, person, place, and activity; ability to maintain meaningful eye contact; appropriate mood and affect; absence of speech and language deficits; presence of social interaction with fellow patients; motivation to get back to previous role; absence of motor problems and physical dysfunction and; absence of comorbid medical condition.
According to Haley & McKay (2004), cooking is the most ideal activity to provide to psychiatric patients especially those with chronic schizophrenia as compared to craft and sensory awareness activities primarily because of the satisfaction it gives to the client. It is very motivating especially to adults because there’s a presence of an end product that is either retained or consumed. It is also age and culturally appropriate and it is concrete and understandable hence meaningful and valued.
Cooking or baking captures the interests of patients and at the same time, targeting improvement of an array of problems and performance deficits. In the case of my client, for example, I preferred to provide cooking as an activity to target her problem areas because she wanted to return to her previous role as a helper, and cooking is just one of the tasks accomplished by a helper.
During the treatment process itself, I was grateful to have learned that my client usually cooks in the ward during OT sessions. It was something she really enjoys doing – cooking and preparing a simple meal and later on, eating and sharing it with the other patients whom she usually hang out with within the ward.
Over all, I used a top-down approach to target my goals. I considered my client’s primary goal to return back to her work and this is what I concentrated on. The intervention method I used was more of a remedial approach since I provided a cooking activity incorporated therein were to target reality orientation and prevocational skills training by focusing on enhancing specific work behaviors that client would need if ever she decide to return to work in the future. I adopted an attitude of active friendliness to establish rapport and to gain client’s trust. Verbal cues prompts and demonstrations were also provided.
My client recognized me as soon as she saw me but she hardly remembered my name. And when she found out that we’re going to cook pudding on that day, I saw that she became enthusiastic about it. She was aware of the need to wash hands and utensils before and after an activity. She was also able to orient self to person, date, place and activity and to time while looking at the clock when asked. She demonstrated good and sustained attention and she was able to concentrate on task throughout the activity. She was able to demonstrate safety awareness while cooking (turning off and pulling the plug of the stove after cooking, and using potholders in handling hot pot and handles). She was able to follow through task with the aid of written and verbal instructions. Client was also able to do aftercare (disposing off garbage and waste products in the trashcan). She generally demonstrated appropriate affect and euthymic mood throughout the activity. She revealed good insight after the session and was able to recall steps in cooking pudding. Client was able to distinguish materials and ingredients needed to cook pudding upon presentation of materials and reading written instructions. Client was able to perform tasks when asked to, given verbal prompts.
During the cooking task, I made sure that all sharp utensils like fork and knife were just within my working area and out of my client’s reach as a safety precaution. I was also the one to open the can of milk for her. Because even if my client appeared high functional, I couldn’t really tell what might happen or what she might do that may compromise our safety and performance of the activity. I also provided a written instruction of the ingredients and the procedure in making pudding. I made sure that the steps were brief, specific and written in tagalog and in larger font so my client would easily understand. At first, she was hesitant about reading it and she told me that she couldn’t read that well. I just pushed her and reminded her that during our first session she was able to read though she encountered difficulty, at least she was able to read. So there, she finally read. I knew it was just a matter of motivation and convincing her, since I think she perceives the task of reading as stressful and requires a lot of processing. There were just instances that she was really having a hard time to read and was taking a longer time in reading and I just gave her prompts to help her. It was either, she really has problem in reading skills, or she was just less motivated to read, or she may have visual-perceptual deficits as well, since she needed to lean closer to read the material. And during the evaluation, she revealed fair performance in the visuospatial task; she needed to turn the paper to complete the figure.
I observed that during the session, her clothes hang loose over her shoulder and she didn’t seem to mind it at all. So even if it wasn’t originally indicated in my goals, I decided to include education on awareness of appearance, of which I received positive response from my client. She became more aware of her clothes hanging loose over her shoulder after reminding her of it twice that even after our treatment session was done, she fixes her clothes whenever it hangs loose over her shoulders.
Client was able to remain sitting and patient while waiting for the pudding to cook. There were very minimal signs of impulsivity (i.e. asking to include all the breadcrumbs to the mixture). She was also able to demonstrate good social interaction with other patients when she decided to share the pudding with them. She even took the initiative to prepare the plates and spoons to put the cooked pudding into after cooking, and asked me to divide it among them. Client was able to wait until the pudding cooled, and listened for my instructions before eating. I also provided additional instructions regarding safety awareness, which had been easily grasped by my client.
Client was able to recall all the steps and the information I told her after the activity, what I just noticed was that, she seemed to dislike the idea of having to process for questions that require her to ponder over. She answers impulsively without taking time to think it over. When I asked her, “do you think we’re going to need this (cheese spread) in making a pudding?” she answered with, “hindi ko alam, ikaw bahala..” She doesn’t seem to like the idea of having to problem-solve; she was too receptive to information. To her it was like, tell me what I need to do and I’ll do it. Hence in her succeeding OT sessions, I would recommend providing her more activities that would target improvement of problem-solving and decision-making skills. Cooking activities may also be done, given she has to cook a variety of dishes graded from simple to complex. Also, SST of buying in the market, education on proper grooming, pre-vocational skills training targeting saving money or marketing and, Discharge Planning and Transition Planning.
At the end of the treatment session, I was really grateful that my client finally remembered my name, and she was able to call me by my name every now and then. I felt glad when after the activity she was constantly thanking me for giving her the chance to cook pudding, which they later on enjoyed eating in the ward. It was fulfilling for her because it gave her the feeling that she made it herself, it came out well and she said that it really tasted good.
When I first got into NCMH, I always thought I wouldn’t make it. I didn’t have any idea how to handle psychiatric patients. I was too scared to face clients with chronic mental illnesses but then, I was glad that I was able to accomplish my three days of fieldwork fulfilled that I thought I had just done what I ought to do. My clinical supervisor told me after the treatment session that I was more at ease and spontaneous during the treatment than how I did during the history taking and evaluation. I guess, indeed I was. Because on the treatment session I already have an idea of what my client is and what I’m planning to do to her. Unlike during the evaluation session when it was almost like I was facing the unknown and I hadn’t the slightest idea of how severe or functional my client will be.
The major difficulty I encountered throughout my fieldwork would be on deciding for my intervention plan. When I decided that cooking would be the most appropriate and suitable activity for my patient, the question that was going on in my mind was to whether they would allow me to cook within the ward. Whether it would be safe to let my client cook, handle cooking utensils and manage a stove. Supposing they’d allow me to cook with my client, what if the other clients crowd around us during the activity? I was also wondering then as to how my client is going to respond to the idea that we’ll be cooking pudding on that day. So on the actual treatment session, I prepared all the materials I will need in making a pudding. At the same time, I planned an alternative activity, which is tuna sandwich making of which I also brought the materials that I’m going to need, in case they won’t allow me to cook with a stove. When the supervisor in the facility told me that I can cook using the electrical stove in the ward, and when my clinical supervisor asked me on which of the two activities I proposed I am going to pursue, I proceeded with pudding-making. For reasons that, cooking is a very motivating activity, I personally love to cook. Second, tuna sandwich making is a relatively very easy step to provide my client, it is not as complex as cooking and it doesn’t provide enough challenge to target a number of skills.
Generally, I could say that I performed well during the evaluation and treatment process. I have targeted most client factors and skills including work behaviors, insights and over all performance in the occupation of cooking and meal preparation. While we perform cooking pudding, client was able to relate previous experiences in cooking in the ward. She also told me that pudding was her favorite food and that she usually asks one of their supervisors in the ward to buy her pudding with her money. I told my client that now that she knows how to cook pudding, she has the option to cook every now and then in the ward or share the knowledge with her friends in the pavilion. But the problem is the opportunity to cook and the availability of the resources. Since client only gets to cook during OT sessions and of which she is supervised. The generalization of skills cannot be promoted and learning cannot be monitored unless a follow-up treatment and re-evaluations will be conducted.
More or less, the fieldwork provided me the experience and the learning I needed in dealing with mentally ill patients. My motivation has always been like, “kung hindi ko ito magagawa hindi ako OT.” But then, the patient I handled was more or less functional already, and not all mentally ill patients would be as easy to handle as such. It really requires a lot of knowledge, experience and competence in this field to not just pull it through but to be empathic enough in understanding the needs and the situation of psychiatric patients. People whom I just usually see roaming around the streets in their rugged clothes and keep me wondering what went wrong.
Reference:
Haley, L. & McKay, E. A. (2004). Baking gives you confidence: User’s views of engaging in the occupation of baking. British Journal of Occupational Therapy, 67(3), 125-128.
*Here are pics during our last day of fieldwork at NCMH in Mandaluyong:
-
First Encounter at NCMH
When I was assigned to conduct fieldwork at the National Center for Mental Health, it was truly a mixture of feelings. I was very excited because that was the first time that I’ll be sent to a psychiatric setting. My previous fieldworks were mostly of adult patients with physical dysfunction and adolescents with mild psychosocial problems, and it was my first time ever to really work with mentally ill patients. On the other hand, I was nervous also. Not just me, but as well as most of us assigned at NCMH because it was our first time to be there. It was also my first time to be in a mental hospital with patients whom I could call really insane. I mean, the typical schizophrenics you would see on the streets – most of which are really chronic in condition.
The first question that I had in mind then was “how am I suppose to deal with these people?” Really, what kind of help do mentally ill patients need? It is really complicated and difficult to imagine how to deal with severely cognitively impaired individuals. Will the goal for treatment would be to get them back to the original level of functioning, or at least near normal?
The patient I observed was having difficulty in organizing thoughts and in social participation. The therapist in charge was using the cognitive disability FOR to teach skills that focus on improving the client’s concentration, frustration tolerance and attention span which were problematic. To achieve client’s goals, the therapist used a stitching activity, which she incorporated in a group session. The intervention technique generally used was restoration in an attempt to target specific client deficits in performance areas, and gradations and adaptations were provided like simpler instructions, designs and materials used. Since the patients in the group were high functional already and are to be discharged in a few weeks time, the approach used was generally top-down so that the skills learned by the clients could be readily applied outside after discharge. Some clients seem to respond very well while some clients seem to challenge the therapist. I guess, you really have to be strong and you must establish authority at the very start of the therapy session especially when you’re working in a psychiatric setting to gain client’s cooperation for a more effective treatment.
-
OT182: work experience
Work somewhat delineates an adult from a youngster. It somehow provides a huge demarcation line between being physically and emotionally mature than being dependent and single-focused students before. Work settings are really a different world from that of the school grounds. Upon entering the grounds of one of the huge export processing zones of the country, I had to admit that I kind of felt strange. It was rather a mixture of nervousness, reluctance, and ironically, sheer excitement. It’s truly a different environment. Anyhow, I’m nervous because I had no idea what to do, what kind of work they’re going to allow me to venture and I never really felt a single streak of confidence or competence at least, for I lack adequate knowledge regarding such work setting. However, this work experience that I had at KAC gave me a wide array of knowledge and new experiences, most especially on the whereabouts in blue-collar jobs such as in a factory setting.
As a part of my work experience, I was initially placed under Warehouse where I get to stack and monitor materials and help in the inventory. I was also placed at the Assembly section where I get to assemble insulators and file F connectors. Work is mostly manual and a bit mechanical in Assembly. I have worked from 7:30 in the morning up to 4:30 in the afternoon with three breaks in between from November 9-11. The first break is at 9:30, in a span of ten minutes; the second one is the lunch break itself at 11:30 until 12:30 and; the last break time is at 2:30 in the afternoon, in a span of ten minutes as well.
In my assigned task at the Assembly, the position maintained throughout the time is sitting, in a folded chair, with the table edge in a height that approximates that of an armrest. While in the Warehouse, more often you are standing and walking around to accommodate the welders and workers’ item requests and material issuance, or your sitting when writing the inventory and reports. Moreover, the use of protective devices was strictly reinforced. In assembling materials, I was required to wear finger cots or cotton gloves, or even an apron, because the materials are greasy and it would be slippery to handle precisely. I was also required to wear an extra clothing aside from the clothes that I already wear because the work is messy and I might stain on my clothes with the cutting oil so I had to change in a white shirt which is similar to the other workers’. In the Assembly, the physical demands of the job include having a good muscle strength of the upper extremities, good coordination, dexterity and hand manipulation. It also calls for an effective bilateral hand use, fine motor skills precise grip and endurance. The task of assembling also requires a good visual figure-ground and visual memory. Psychosocial demands include good orientation to time, person, place and event, and good concentration. Sustained attention and effort, and good problem-solving skills should as well be better established. The task is mostly individualized and there is minimal contact and interaction among other workers and with the manager unless if you have inquiries or complaints.
During my entire 20-hour work experience at KAC, I was convinced that working in a manufacturing firm or any factory for that matter is twice as complex as we would perceive it to be. I have worked in a variety of job settings but most of which involves clerical task assignments unlike when you were integrated in a work area where you can really literally sweat it all out. Although being assigned at the Warehouse, or at the Assembly section, or at the Production office didn’t give me as much utilization of manpower as to that of the machine operators, I could still call it a physically challenging experience. Like for example, when I assembled the insulators for the F connectors. At first I thought it’s as easy as this-then-that and voila, there you have the insulator. Then again, the task of course requires good hand dexterity, a fully functioning vision and good eye-hand coordination, and most importantly, effective bilateral use of the hands. The task is also repetitive so as I was getting on with the task, I’m beginning to feel some muscle strain on my elbow and shoulders. In addition to this is the static posture of the body in sitting that contributes to strain and eventual pain at the back. So it is really worth noting to take a rest once in a while so as to not force yourself to the limits.
Next was when I was allowed to file the assembled F-connectors. The task requires a well developed fine motor skills and precise pinch grip. It would put a strain in the elbow flexors, occasional strain at the back and paresis of the fingers and hands if short breaks to rest were set aside and ignored. Amidst all this, it is not only the physical demands of the job or the physical capacities and skills of the workers that affects the job performance. Psychosocial factors such as the worker’s relationship with the employer and with the other workers could as well impact on the engagement of occupations in a job setting. It might as well pose as an occupational hazard in the work environment. With regards to my experience at KAC, I had not a single problem when it comes to getting along and interacting with the other workers or with the managers. I was thankful enough that all the people there are very friendly and accommodating. They indeed facilitated in my course of learning. Of course it is not unusual that in any work setting there may be issues among the workers but this condition is only triggered if the members of the company – workers, leaders, managers, employer, has no clear and open communication among each other. Another factor is the work environment itself. I must admit, sometimes it really disturbs me to hear all the noises coming from the machines. Anyway, it would be impossible to be working in a manufacturing firm plus all of the machines being operated without a single noise being produced.
All in all, being integrated in an actual work setting gave me at least the knowledge on the workers’ welfare in such field. I was able to observe and experience first hand the existing physical demands and occupational hazards in a manufacturing industry; and even the process on how the automotive and precision parts are manufactured step by step. Even though I had a difficult time in pursuing this work experience, I must say, it’s all worth it and I’m thankful that I did. Now I know how hard it really is nowadays to actually seek for a job.
**This is just an overview of my entire Job Site Analysis.. I just wanted to provide a glimpse of what I had gone through and the experience I had this past semestral break. ^_^ -
OT100 Disability Day Report: Trying on Someone Else’s “Imperfect” Shoe
Being a handicapped person or someone who has a disability is very difficult, even more when you have to live with it. You get ridiculed and ignored as if you have been trying to spread a plague whatsoever. People may be kind to those who are or who have been disabled physically but it is the ones who have mental illness who were often rejected and misunderstood. This is what I had to go through during the OT100 Disability Day last July 11, 2005 from 8 in the morning to 12 noon as I tried to simulate a person with mental and/or behavioral illness. Four hours of enduring an intricate task which had enlightened me and made me realize that though some individual may be different, still, we all are the same – we are human beings created by God.
My assigned disability was Attention Deficit Hyperactivity Disorder (ADHD). This disorder occurs mostly during childhood and if not treated at early age might continue until adulthood. Among the common manifestations of this disorder are: inattentiveness, impulsiveness and hyperactivity. A child with ADHD has poor memory, poor communication skills, hyperactive and acts without thinking. He is restless and finds answering homework far more difficult than other children. He cannot focus on one task for long for he easily gets bored and impatient. He also has the tendency to develop other disorders such as bipolar disorder and conduct disorder.
Since I was simulating an adolescent with ADHD, I had first conducted a mini research on how this kind of disorder manifests among teenagers of my age. Definitely it would be a lot different in adolescents than that of children. And I learned that the degree of hyperactivity sort of decreases but evidences of poor attention and slow mental capacity is still present. So I planned early on how I am going to simulate the disability and listed down some activities or acts I could perform on the disability day per se, like always fidgeting on my seat during our ride on the jeepney and never seeming to stay in one place, inability to stare and focus on anything for a long time, not paying attention when someone will talk to me and avoiding eye contacts, pointing at objects that will catch my attention, blurting out random things, doing this mannerism of twitching my face I devised myself etc.
The place where I had to simulate my assigned disability was at Isetann Recto. The general status of people there was that of “middle class”. There are a lot of vendors, workers and some students. They wouldn’t actually throw violent reactions at me since I was wearing the typical shirt and jeans of a teenager and I am cleaner as compared to my other block mates who were simulating people with bipolar disorder until I would show some signs of “weirdness” that they’d look at me in annoyance or they’d laugh at me. Because they had no idea what I am going about and I doubt it if they even know what ADHD is, they’d just simply turn away not seeming to care or they would stare at me as if I had the strangest look in the world!
Mostly, the students or the people of my age were the ones who are less understanding. There is this one guy I asked for direction and when he’d started talking I tried not to pay any attention pretending I saw something strange in the sky, then he uttered, “may diperensya ata ‘to eh”. And his entire friend laughed. While we were on the jeepney, I began my “theatrical act” of restlessness, trying to appear impatient and irritated, and all the people inside the jeep looked at me with question marks on their faces, while some are already getting irritated with me. However, there is this one woman I encountered whom I could never forget. I was about to cross the streets, and she too. When there were no other vehicles that seem to pass by and the road was free for the pedestrians, she must had noticed me somewhat unaware of reality that she decided to pull me by the arm to cross the streets with her. It was really nice for her to do that.
It was really a different feeling to pretend as someone whom other people think of as less capable for a person. Though majority of the people were indifferent to people with disabilities most especially with those suffering from mental illness, there are still few who were kind enough to even ask what’s wrong with me and it made me feel that somehow there are still some who are willing to care.
One of the difficulties I encountered during our Disability Day was how to make other people notice me and to convince them I have ADHD. Almost everybody thinks of insanity as a generic for all mental illnesses regardless of whether it is schizophrenia, bipolar disorder, depression or mania. Another thing is that, people with ADHD have the tendency to develop conduct disorder and manic-depressiveness, so it was certainly a challenge for me to think of acts where in I could show manifestations of ADHD in me and at the same time, staying out of trouble. So I just tried to do acts that are a little bit more discreet like trying to enter at the exit gate of Isetann, getting hold of some items in the store for a long time but not to the point of putting it to my pocket and though I blurt out random words, I tried not to scream foul words.
The accessibility of the place in relation to people with ADHD, I believe, is fair since people with ADHD are not as dirty-looking as those who are severely affected by disorganized schizophrenia and bipolar disorder. They even get to study and work as normal people do. More often than not, ADHD in teenagers is not that obvious than that in children. I easily got inside the mall, and even my other block mates who almost seemed like taong grasa as they simulate people with bipolar disorder. But the amount of support people with mental illness get is relatively few as compared to that of the people with physical disabilities because they are often misconceived as dangerous. They are the ones often marginalized by the society, and even if there are institutions that are willing to help them, there is not a single person willing to put them in.
People with disabilities deserve proper care and respect. Yes, they may not be able to do what others can but this does not permit us to laugh at them, call them names or to stay away from them but instead do something to help them. I, as a student, may not have that much of help and support to provide them but I could start off by educating other people around me to avoid further misconceptions and discriminations to PWDs. I believe education is a vital tool for understanding. And by learning how these people go through life’s indifferences, we could then help them cope with life better.
It is funny how I used to tell my friend whenever we see the woman with a mental disorder in front of the Department of Justice how I wonder what people like her think and feel, how they became like that and what they are like before they lost their sense of reality. Now, I had at least some idea about their situation by experiencing to be one during our last Disability Day.
The OT100 Disability Day is indeed a very worthwhile activity. It may be a pre-requisite for a major subject in college I am taking up right now but it also provided me the knowledge about people with disabilities and thus made me appreciate Occupational Therapy more. It helped me realize that I am on the right track all along. This activity helped me understood more about PWDs most especially those with mental illness. I understand now that they need care and support from the environment and from the society to at least live as normal people do, for to be able to understand other people around you means being on the other person’s shoe. And this made me decide to pursue OT to be able to help these people.
This activity had been very meaningful for me in studying other people with disability. It can be improved more if a student was put in a variety of setting during the simulation to elicit different reactions of people from different statuses. I had a lot of fun and I learned so much from the activity. It was in fact the strangest yet most fruitful four hours of my life.
Ma. Joanna B. Torres
2004-36778 -
OT 101
What the heck is an OT???
This is what I told my self before having any knowledge of it...
At first, when I was still writing down the course I would like to enroll in college. My first choice was of course, the ever in-demand "BS Nursing"... yeah, just because of "parents-told-me-to" thing...well, I didn't personally like it. What I really wanted to take in the first place was electronics and communications engineering...or something which has to do with interior designing stuff...but I bummed! Instead, I wrote nursing as a first choice...and....BS Occupational Therapy as my second choice in the most prestigious premier state University of the Philippines. Why? My friend told me it's good... and because my sister needs special care...from an OT that is, so I wanted to help her...hopefully...someday. (Though it was just my second reason at first)
Occupational Therapy is a field ...uhm... let's just define it this way.
These are some unique definitions of OT that I came across in the net:
"A physical therapist will teach you how to walk; an occupational therapist will teach you how to dance"
"How many OT does it talk to light a bulb? None. The occupational therapist will teach the bulb to light itself"
And the ever famous proverb that is most apt to define what an OT does:
"Give a man a fish and you'll feed him for a day; Teach a man how to fish and you'll feed him for a lifetime"
Pretty inspirational stuffs huh? Why am I telling this to you? Well, why don’t you ask yourself first... why are you reading my post anyway? But since you're reading it already... Im not in the position to give you the correct definition of an OT nor am I a professional in this kind of field... oh yes! You heard it right; I enjoy being an OT now!!!!!! Unbelievable? he he...it’s because OT is the most wonderful job there is!!! Let me tell you bout my past experience so you'll understand.=)

On the 6th of April 2005, we were asked to do this observation for an OT clinic as a pre-requisite for a major subject we are going to take in our second year in college that will last for about five days. At first, I was reluctant about it…I thought it would be boring and all but...it was fun! It was rather great!
My first observation was with this little girl…she has ADL (im not sure) and she was all this dizzy all the time as the therapist guides her and teach her how to grip a spoon, put the food on her mouth and chew it…yes, you read it right, step-by-step. I was pretty amazed by how patient these people (the therapists) are, despite the children’s whining, throwing everything their hands got to touch, crying biting, and occasional uncooperativeness…he/she remains patient and loving but firm.
The second one is with this little kudos having an ongoing toddler’s class or something. They said it boosts their socialization skill and participation as a group. But there is this one child that the instant he entered the room…he started crying and crying that he’s unstoppable! So the other kids go on crying too. And when I gazed outside to see the parents peering through the glass door, some of them were crying as they watch their little ones…I was deeply touched. It was so much a burden for the parents to see their child suffering; unaware of the reality they’ve been going about. And during this pre-play session that we got to participate in and even played with the kids…there is this one child that I could never forget. The therapist told us that he (the kido) whenever roams around the mall or somewhere with his parents…he’d go to the prettiest girl on that place and would hold her hands, and he especially like kissing people. And all the while, during the entire session, he would always turn to his back (where I was) and would blow kisses at me. Or he would climb down his armchair and would kiss my cheeks. So sweet. He even calls himself, the “kissing bandit”. And before the therapy session ends, he told me, “go to my house, play with my toys”. Awwww….sweet! little angel.=)
And everyday, during our observations, I’ve witnessed a lot of activities and kinds of therapies the “teachers” employs to these little kids. Mostly concerns the child’s Sensory Integration, Motor Planning and Socialization Skills. Oh, heck! I’ll learn more about that in my second and third year.Ü and I think, now, I’m already ahead with my classmates! Coz I’ve already learned a lot of things about what an OT is through this observation thing…

When you’re handling a child…no matter how smarty-pants you are back in college with all these terms you memorized in your major subjects…it is less likely useful. I mean, I’m not saying that it won’t matter….it will. It’s just that, no matter how much you know about occupational therapy, still, it’s different strokes, for different folks, in this case, when it comes to the patients. Though special children deserve special care, what you are trying to impose upon them is a world like that of normal children. So you must learn how to establish rapport, when to be gentle and when to be strict. You shouldn’t let the child control you that you’ll give in to his demands so he’ll follow you…you have to show him who’s the boss. I’m not saying it’s about building tyranny or whatsoever over the kids, it’s a matter of teaching them and making them realize that not all the time they’d get what they want. They should learn how to wait for their turn, wait for the instructions of their teachers or parents before doing anything, be independent and learn how to listen and pay attention. And this goes to “normal” kids as well.
This 5-day observation changed my life entirely…
I finally realized that I’m on the right track all along. I wanted to be an OT someday. Not because of the extra high salary…of course I admit, it was a part of it. More importantly, I want to help these young people. I want to be a part of their lives. I admire the OTs who never seems to get tired of molding the lives of these young and innocent children that are “uniquely” different that makes them apart from the rest yet special and indeed, smart individuals who are also a part of this world. I hope that people wouldn’t look down on them (special kids with CP, ADHD, DS etc.) anymore. That they’d think they are hopeless because of their sickness and that they are burdens of the community. You know what I think about the people who think this way? They are the real hopeless ones. They are the real burdens of the community. Because though normal, they couldn’t be effective individuals in their own ways. Heck, they’re just wasting their lives!
Being an OT entails so much responsibility. Coz you are like the second parent of your patients. The parents would trust you with their little ones and these little “special” ones give you the same amount of trust and love as well. So an OT, is not just a course mastered, it’s a matter of commitment and dedication. An OT is not made; he is born. And he’s probably the most compassionate being there is. How I wish I could be a good OT someday. I want my patients to love me too, I just love children and I love seeing those happy faces staring back at me.
“Choose a job that you love and you never work for a day”
That’s what we should always bear in mind. So we’ll never regret anything at the end. And I assure you, you wouldn’t enjoy being an OT if you don’t love it and just go for the money.
And you know the best part of it…? YOU GET ALL THE HUGS AND KISSES THAT YOU WANT! Well, from the kids, that is.=)
Anyway, I hope you enjoyed reading my article as much as I enjoyed typing it. Ta ta for now! (~^.^~)



